Successful Closure of a Large Thoracic Aortic Aneurysm
We are happy to inform you that we performed percutaneous closure of a large thoracic aortic aneurysm recently at our hospital with excellent results. A patient is a 65-year-old man, a reformed smoker, diabetic and hypertensive. He underwent coronary bypass surgery 6 years ago. When he went to a physician for breathlessness on exertion. Suspecting COVID, the doctor advised a CT scan chest. There was no COVID pneumonia but a large thoracic aortic aneurysm was diagnosed. After consulting at different hospitals, he finally came to us. The CT also showed that all his bypass grafts were working normally. Echocardiography demonstrated that his LV function was normal.
CT findings in detail: The aneurysm started after the left subclavian artery. There is a healthy zone of about 1.5 cms length after left subclavian origin so there is a good landing zone for placing the uncovered portion of the device. The length of the aneurysm is 6 cms and the diameter is 6.0 cms. There is a huge layered clot inside. Luckily for him, there were no branches of significance coming close to the aneurysm. There is once again a landing zone of several centimeters between the aneurysm and the coeliac artery origin.
Plan: The treatment of thoracic aortic aneurysm could be surgical or percutaneous closure using a stent graft which is a high profile self-expanding Nitinol stent over which a cloth-like material is stitched to prevent the blood from leaking into the aneurysm effectively sealing it. In view of its large profile, there is a need to surgically expose the iliac artery and after the procedure is over to repair it. The post-procedure patient needs to be on dual antiplatelet therapy for a prolonged period of time. Expenditure is more with intervention but the risk is less and the procedure is more patient-friendly so much so that many surgeons also adopted it.
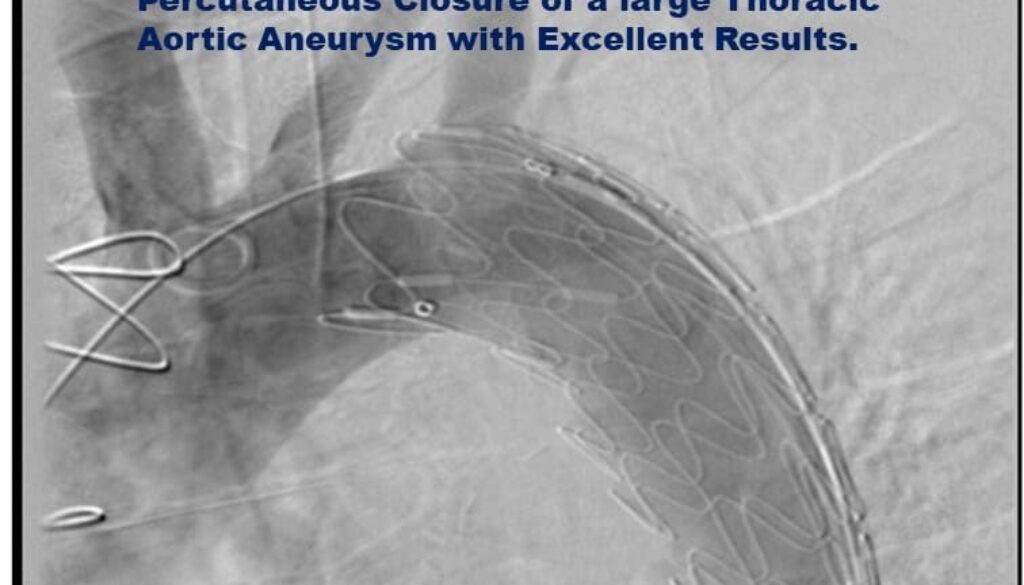
Procedure: We implanted a 32mm× 80 mm device distal to the left subclavian artery. Dr. Ravi Raju did the dissection of the groin and exposed the right common femoral artery. The critical care team helped us by giving the required anaesthesia. The patient got discharged the next day. The pictures are enclosed.
Natural History: Thoracic aortic aneurysm is a critical condition and carries huge mortality. The epidemiology of TAAs is challenging to study because it is a clinically silent disease. Approximately 60% of TAAs occur in the root or ascending aorta, 10% in the arch, 40% in the descending aorta, and 10% in the thoraco abdominal aorta; however, an aneurysm may involve multiple aortic segments. TAAs are asymptomatic in >95% of cases. Most TAAs remain undetected unless incidentally discovered as in our case. In addition, many fatal TAA ruptures or dissections are misdiagnosed as myocardial infarction, thereby underestimating the true prevalence of TAAs. The prevalence of asymptomatic TAAs has been reported to vary between 0.16% and 0.34%. The annual incidence of TAAs has been assessed at approximately six to 10 cases/100,000 patient-years.
Biomechanical studies have supported clinical findings of 6.0 cm as a dangerous threshold. The average ascending aneurysmal aorta expands by 0.10 cm annually, whereas descending TAAs grow by 0.29 cm annually. Aneurysms with larger diameters tend to grow more rapidly. Given that the 5-year survival of untreated TAA >6 cm falls to 54%, it is important to diagnose and treat these cases. Certain categories of patients need screening like octogenarians, relatives of known cases of TAA, patients with Marfan syndrome, and those who had a history of cerebral aneurysms.
Follow-up: Our patient did very well and has completed 3 months of follow-ups.