Interesting Case done at Indo US Superspeciality Hospital, Ameerpet, Hyderabad
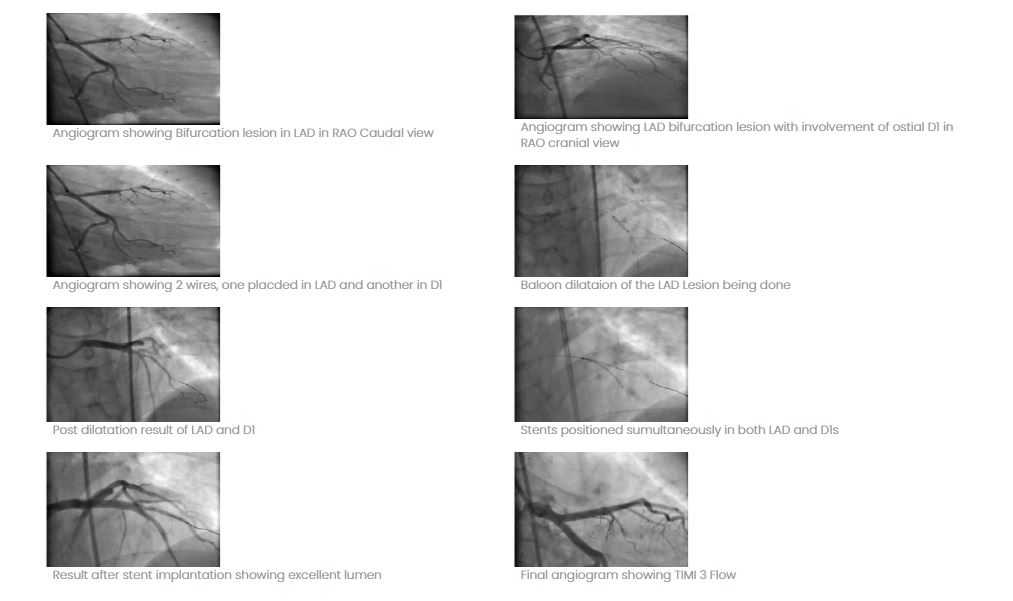
At Indo US Hospital, we have recently performed a case of complex angioplasty by a relatively new technique called “SKS” (Simultaneous Kissing Stents). A 40 year man presented with unstable angina and angiogram showed a critical lesion of LAD (left anterior descending Artery) involving the bifurcation of LAD and large diagonal. After dilating both the vessels, 2 stents were simultaneously placed and implanted with excellent result. This technique is called “SKS” technique. This technique is used less often but if properly done gives excellent long term results. We have done it in 8 cases in the last 6 months and all of them are doing well.
- Case Study 1
- Case Study 2
- Case Study 3
- Case Study 4
- Case Study 5
- Case Study 6
- Case Study 7
- Case Study 8
Interesting Case done at Indo US Super speciality Hospital, Ameerpet, Hyderabad
At Indo US Hospital, we have recently performed a case of complex angioplasty by a relatively new technique called “SKS” (Simultaneous Kissing Stents). A 40 year man presented with unstable angina and angiogram showed a critical lesion of LAD (left anterior descending Artery) involving the bifurcation of LAD and large diagonal. After dilating both the vessels, 2 stents were simultaneously placed and implanted with excellent result. This technique is called “SKS” technique. This technique is used less often but if properly done gives excellent long term results. We have done it in 8 cases in the last 6 months and all of them are doing well.
We are presenting an interesting case in which thrombolytic therapy was used for a totally occluded vein graft presenting as acute myocardial infarction. Mr. JR, 75 year old has presented with chest pain for 2 hrs. He underwent CABG 10 yrs ago. The ECG showed acute inferior MI. Echo showed good LV function (EF:50%). He was taken up for primary angioplasty within 15 minutes of arriving at Indo US Hospital. He was given a loading dose of 2 tabs of Ticagrelor and 150 mg of Aspirin. His native coronary angio showed triple vessel disease.
The LIMA to LAD was normal. The vein graft to right coronary artery was found to be totally occluded and we diagnosed that this was the culprit vessel causing the MI. After crossing the occluded vein graft with a guide wire, a thrombus extraction catheter (EXPORT) was passed several times across the lesion and large pieces of thrombus were extracted. We saw that there is a severe obstruction in the middle of the graft which was causing this problem and a stent (4.0×24 mm) has been placed at the same point. At this stage only transiently flow was established in the vein graft. Several vasodilators were given into the graft to establish distal flow but without success.
Hence it was decided to give intra graft thrombolytic therapy using streptokinase. 100000 units of the drug were given and the patient was shifted to ICU. The remaining drug was given over 1 hour intravenously. Patient had complete resolution of chest pain and ST elevation. The femoral artery sheath was left in situ and a repeat angiography done after 24 hours showed excellent patency of the graft with TIMI Grade 3 flow into distal RCA. The case illustrates the role of thrombolytic therapy in vein graft intervention in a case of acute MI. Our patient did not have any complications like bleeding at the puncture site in the right groin. He is doing well with excellent LV function.

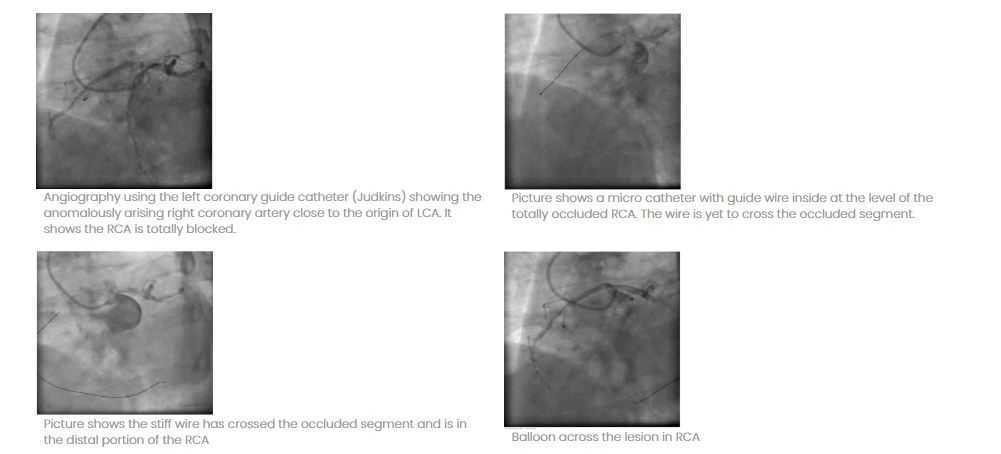
CASE OF CHRONIC TOTAL BLOCK OF AN ANOMALOUSLY ARISING RCA SUCESSFULLY SUBJECTED TO PTCA
Mr. M. aged 52 yrs, diabetic on oral anti diabetic drugs has come with class II angina for 6 months. No history of myocardial infarction in the past. The treadmill test was positive. His Echocardiogram was normal and coronary angiogram showed normal left coronary artery but the right coronary artery could be found only with difficulty as the vessel was arising anomalously from the roof of the left coronary sinus draining in the AV groove, and was found to be totally blocked (It was going behind the aorta). A decision was made to open the complete occlusion of the right coronary artery.
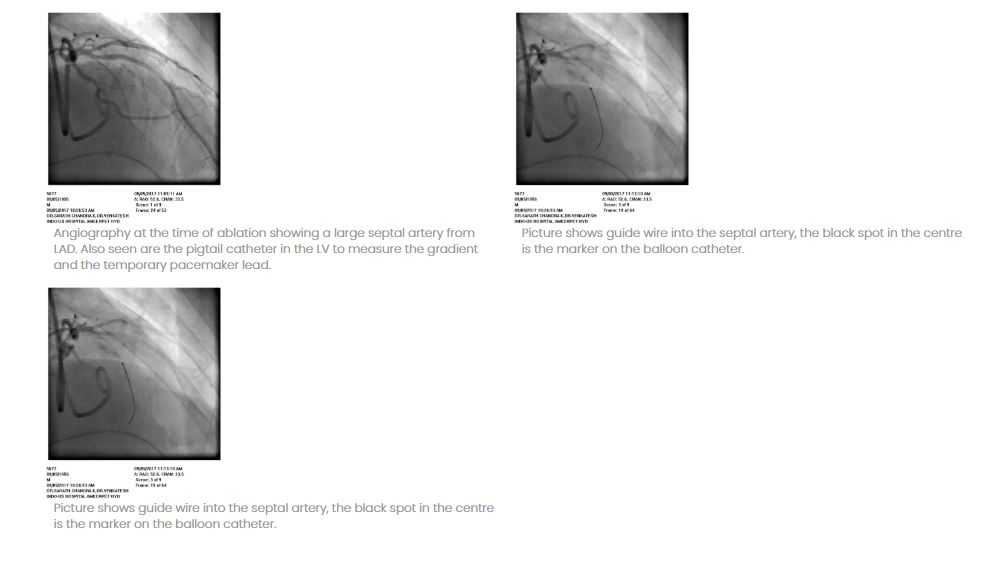
Case of Hypertrophic Cardiomyopathy treated effectively
Mr. R, a 57 years old male has come to Indo US Hospital, Hyderabad with recent onset of breathlessness on exertion NYHA class II. He gave history of atypical chest pain for about six months. There was history of near syncope on exertion twice in the last 6 months. He is a diabetic for the last 15 years but did not give history of Hypertension. He is a non-smoker and Teetotaler. He was evaluated at Nellore and was diagnosed as a case of hypertrophic cardiomyopathy and was advised to undergo alcohol septal ablation for which he was referred to us. His physical examination showed a prominent LV type of apex with palpable S4. There is a systolic murmur of 2/6 at left sternal edge. His BP was 130/80 mm/Hg, heart rate 84/min. There were no sign of heart failure. His electrocardiogram showed RBBB with left atrial enlargement. chest x-ray showed mild cardiac enlargement. Echo showed severe hypertrophy of left ventricle which was assymmetric indicating that the intra ventricular septum hypertrophy is more than that of the posterior wall (unlike simple hypertension where the hypertrophy is symmetric). The IVS thickness was 19 mm and PW thickness was 15 mm. There was SAM (systolic anterior motion) of the AML (anterior mitral leaflet). There was a gradient of 140 mm in the out flow tract of LV, due to obstruction just below the aortic valve produced by SAM.
There was mild mitral regurgitation. With this data it was quite clear that we are dealing with a case of severe HOCM. In view of his symptoms, we decided to do Alcohol septal ablation. Coronary angio showed normal coronaries. The LAD has a large septal artery which is conducive to alcohol septal ablation. The septal artery has been wired and a 1.5 mm over the wire balloon was passed into the septal artery and the balloon was inflated. The wire was then removed and 100% (absolute) alcohol was injected at 0.5 ml at one time to a total of 2.0 ml. The gradient has come down markedly in the next few minutes. The whole procedure was done under echocardiographic guidance. A temporary pacing wire was kept starting from the beginning of the procedure till 48 hours because there is a small risk of complete heart block. No adverse effects occurred in our patient and he recovered uneventfully with nil gradients at the end of the procedure.
The alcohol when injected into the septal artery produces a controlled small infarction of the basal septum and their by relieves the obstruction. The procedure is now fairly standardized and safe. A small number of patients may develop complete heart block and may require permanent pace maker implantation. In our case the result was exceedingly good and echo done at four weeks showed no evidence of intra ventricular obstruction and rhythm was sinus. The idea of presenting the case is to highlight the importance of this relatively new mode of treatment in an important group of patients. With the advent of alcohol septal ablation, the earlier treatment of surgery namely surgical septectomy has nearly become extinct.
Mr. A, a 67 years old male has presented with angina for the last one year. He is a diabetic and hypertensive. He is a smoker. His ECG showed old anterior wall MI. Echo showed good LV function. The angiogram showed diffusely calcified LAD with multiple blocks with several sights of 90% stenosis in proximal and mid LAD. LCX and RCA are normal. In view of his symptoms and diffuse calcification of LAD it was decided to do Rotational atherectomy of LAD. Rotational atherectomy, also called Rotablation, is a fairly old technique.
It was initially quite popular but fell out of favour as it was considered difficult to perform and now has picked up due to fine tuning of the equipment as well as technique. Basically it contains a rotating diamond studded elliptical metallic structure called the Burr. It is rotated at a very high speed of 1.5 to 2.0 lakh rpms. It goes into the coronary artery and cuts away the hard and calcified plaque and opens up the lumen. After that angioplasty can be done like any other case.
Who are candidates for Rotablation? Usually the cases where vessel is densely calcified like in our case, because it is difficult to dilate these vessels with a routine balloon and the balloon will end up bursting and also the stent may not expand. Our patient who had a densely calcified long lesion in LAD underwent Rotablation with excellent result.

ANGIOPLASTY IN THE VERY OLD
Should age be a deciding factor for treatment?
We bring you details of a recent angioplasty done at Virinchi Hospital, Hyderabad. Team Cardiology performed angioplasty for a nano-generian (94 years old) presenting with acute coronary syndrome.
Mr RSR is a pleasant 94 year old man who presented with acute chest pain 6 hours before coming to Virinchi hospital. He is hypertensive and non- diabetic. He is a chronic smoker. six years prior to this event he was subjected to coronary angiography and angioplasty but was told that the procedure was not successful .No records of the procedure are available. His ECG done before coming to us showed marked ST segment depression which improved by the time he reached us. His troponin was positive and echo showed normal LV function. Coronary angiography showed triple vessel disease. In view of his age and frail status it was felt that he is a better candidate for PTCA than CABG. The same was done by radial route with extreme care to avoid excess contrast usage. Patient recovered very well with no rise in serum creatinine and he was discharged in a fit condition on the third day.
What is unique about this case?
These patients are very frail and hence extreme caution is needed while handling such cases.
These patients are otherwise not suitable for surgery, that leaves only angioplasty as their option for revascularization.
These patients usually have reduced renal function .Angioplasty should be done using minimal contrast (this patient’s complex angioplasty was done in 100 ml).
Radial procedures are preferred in these patients as femoral procedure predisposes to groin hematoma.

Patients of coronary artery disease who undergo bypass surgery do well but due to the very fact that their longevity is prolonged they are also prone to develop further lesions in both native vessels and the bypass grafts. The arterial grafts particularly left internal mammary is generally resistant to new lesions and the only problem it faces is an occasional case of distal anastomotic site stenosis.
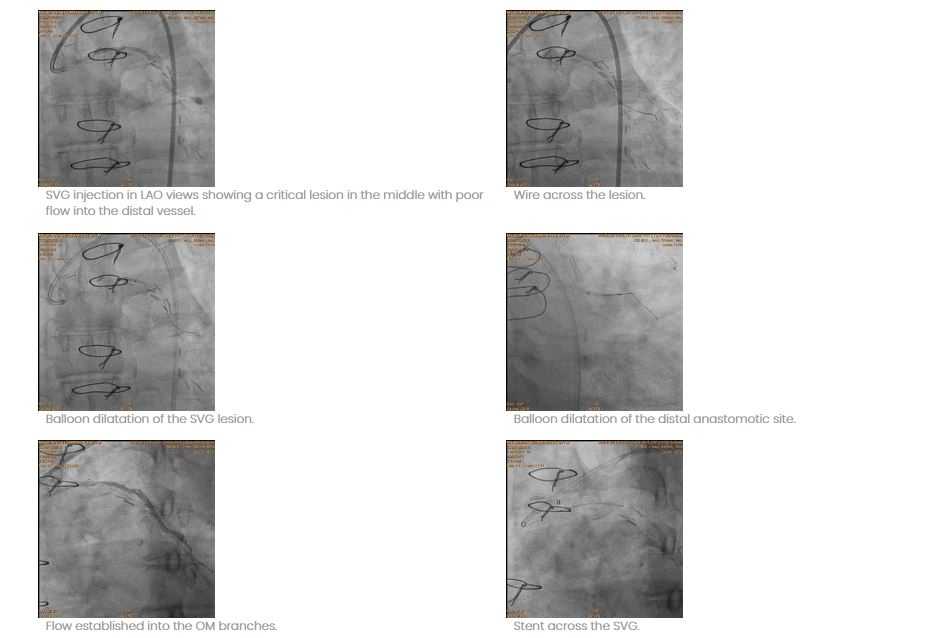
The saphenous vein grafts are prone for occlusion and new stenosis. It is reported from the Montreal study that 15 to 20 percent of SVG s occlude in the first few weeks after surgery. There after they have an attrition rate of 2% per annum in the first five years and 4% per annum in the next five years so much so that at the end of 10 years, 50 % of vein grafts get occluded. The lesions that develop over years in vein grafts are different from the native vessel atheromas because they can be bulky, rarely have calcium and can have necrotic element in the centre. The lesion can have cheesy material that can embolize distally. For these reason a stent should be implanted with caution. For this it is preferable to take a slightly bigger stent than the apparent size of the vessel and implant at a low pressure. We have done an interesting case of vein graft angioplasty a few days ago which we would like to share with the readers.
Mr. SR a 57 year old man presented with acute recurrent chest pain for one week before presentation. The pain was typical and was precipitated by walking, more so after food. He underwent CABG 10 years ago and received several grafts to LAD (with LIMA), SVG to RCA and OM branch and to a large diagonal. His LV function was good and cardiac enzymes were negative. The angiography showed two critical lesions in SVG to diagonal. In addition there was a near total occlusion of distal anastomotic site. We performed angioplasty of this case using a 7 f guiding catheter and a whisper wire. After pre-dilatation with a very small balloon further low pressure dilatation was done with a two mm balloon. The distal site lesion was also opened and good flow was established.Then only the body of the SVG was stented at just 6 ATMs pressure. The distal site was left without stenting as it is well known that SVG distal anastomatic site rarely develops restenosis. He was given vasodilators into the graft. The end result was very satisfactory, no ECG changes and patient recovered very well.
Conclusion: the vein graft disease has to be dealt with great caution and it is possible to achieve satisfactory result.
Mr. V. 75 year old man has come to Virinchi Hospital, Hyderabad with recent onset angina. His angiography showed critical lesions in RCA. There was heavy calcification at the site of the stenosis. As the procedure of angioplasty would have difficulties if this case is routinely done, he was subjected to Rotational atherectomy. This involves using a high speed burr which has micro diamonds attached to its surface which will enable the equipment to cut the calcified part of the atheroma. After doing this, further dilatations were done and 3 stents were implanted in the RCA. The patient improved smoothly.
